Semen Analysis
A semen analysis is the key test for investigating male infertility.
It is performed in compliance with the principles of the World Health Organization (WHO), provides a basic overview of the semen and, at times, highlights whether further special tests are required. It helps the doctor determine whether the male factor is the cause of the couple’s infertility, while it often identifies the fertility treatment that needs to be followed to achieve pregnancy.
Tests
Macroscopic Semen Exam
Semen Volume
According to the reference range, semen volumes ranges from 1.5 ml to 5 ml after 2-5 days of sexual abstinence. It examines cases of hypospermia, hyperspermia and aspermia linked to pathological conditions.
Liquefaction / Viscosity / pH
Sample liquefaction should occur within 60 minutes from ejaculation, while the pH must be higher than 7.2. Viscosity should not be high 20 minutes after ejaculation. If these are not within the normal range, this indicates a pathological condition, usually inflammation and/or glandular disorder.
Microscopic Semen Exam
The following parameters are examined during a microscopic semen exam:
Sperm count
Sperm concentration should be equal to or greater than 15 million per ml, and equal to or greater than 39 million in the total ejaculate. Cases of azoospermia, oligospermia, cryptospermia and polyspermy are examined through further testing, so as to identify the cause and treat them accordingly. Usually, in cases of low sperm count (oligospermia or cryptospermia), cryopreservation of the sample is recommended.
Sperm motility
According to the reference range, total progressive sperm motility, i.e. the sperm that is able to travel to reach the egg, should be equal to or greater than 32%. Low motility may be due to inflammation, structural sperm abnormalities and presence of increased oxidative stress.
Sperm morphology
According to the strict evaluation criteria for sperm morphology laid down by Tygerberg, the percentage of sperm with normal morphology should be equal to or greater than 4%. Morphology plays a significant role in fertilization, as the sperm and the egg should fit together like a lock and key. Low morphology has a negative effect on normal fertilization.
Sperm vitality
This test assists in the further evaluation of sperm quality. The test should be performed on samples with a high rate of immotile sperm or completely immotile sperm, as it provides crucial information as to the existence of live sperm, which, though immotile, may be used for fertilization using the ICSI method.
Other cellular elements
The presence of other types of cells apart from sperm (round, epithelial, etc.) is examined.
Immunology Testing
(agglutination, antisperm antibody tests)
Immunology testing includes an exam that tests for the existence of antisperm antibodies in semen, by identifying two of the most significant of those, IgA and IgG, which are the cause of infertility and inability to procreate. This information can lead to the treatment of the problem, either with pharmaceutical treatment or with the most suitable assisted reproduction method.
Preparation
Before the semen analysis, your treating physician will tell you about everything that needs to be followed as part of your preparation for the test. For accurate results, it is important that the patient follows these instructions:
- Practice sexual abstinence for 2 to 4 days (unless instructed otherwise by the treating physician).
- Ensure he has not had high-grade fever in the last 2 months.
- Avoid alcohol and caffeine consumption.
- Tell the doctor if he is on any medication.
Procedure
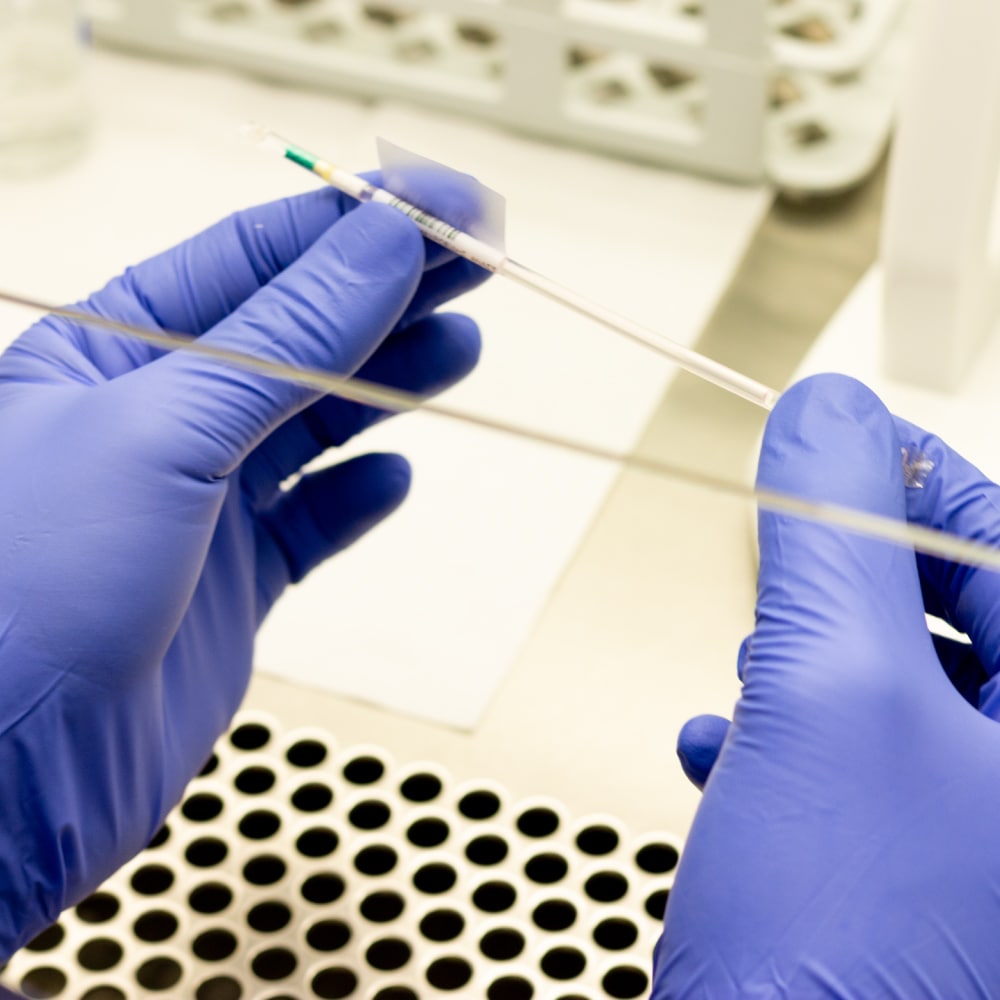
The semen sample is collected in two ways:
- Via masturbation (it is considered the best way for sample collection, without the risk of contamination or loss of part of it)
- Through intercourse, using a condom that does not contain spermicides
If the sample is collected at the patient’s premises, he must make sure that he:
- Uses a sterile urine container.
- Transfers the sample close to his body so that it maintains the body temperature (37°C) as much as possible.
- Transfers the sample to the lab within 45 minutes from ejaculation at most.
- Collects the entire quantity of the sample, without missing part of it.
Results
The semen analysis results may indicate the following.
- Aspermia: Absence of semen
- Azoospermia: Absence of sperm in the semen
- Oligospermia: Sperm count lower than 15 million per ml
- Severe oligospermia: Sperm count lower than 5 million per ml
- Asthenospermia: Low sperm motility
- Teratospermia: High percentage of sperm with abnormal morphology
Pathological findings after a semen analysis may be due to one or more of the following reasons:
- Reproductive tract infection
- Viral infections
- Hormonal imbalances
- Chronic diseases
- Genetic disorders
- Exposure to radiation, chemotherapy or toxic substances (smoking, drugs)
The doctor will recommend a repeat semen analysis immediately, if the results are disconcerting, or a little while later, usually 2-3 months, in all other cases. On many occasions, the test needs to be repeated a few times to get a reliable overview.
Relevant Topics
-
Azoospermia / Retrograde ejaculation
Azoospermia / Retrograde ejaculation During retrograde ejaculation, the semen travels into the bladder and, as a result, the man...
-
Innovative lab techniques
Innovative lab techniques The causes of male infertility are addressed and the chances of success are maximized, based on...
-
Ultrasound
Ultrasound It is often used to diagnose the causes of male infertility, but also problems linked to male sexuality....
-
Genetic Testing
Genetic Testing The advancements in molecular biology and genetics offer the possibility of examining the genes involved in sperm...
-
Hormone Testing
Hormone Testing A hormone test is a blood test that measures the levels of hormones, which play a major...
-
Investigation of male reproductive tract inflammation
Investigation of male reproductive tract inflammation If the semen analysis indicates an infection (increased number of round cells, mucus,...
-
DNA Fragmentation Testing
DNA Fragmentation Testing DNA fragmentation assay is the most important sperm function test. DNA fragmentation assay is the most...
-
Microbiological and Biochemical Analysis
Microbiological and Biochemical Analysis Microbiological analysis is recommended when there is a history of inflammation or indication such as...
-
Sperm activation / Sperm viability
Sperm activation / Sperm viability The total number of progressively motile sperm after sample treatment is calculated. The most...
-
Semen Analysis
Semen Analysis A semen analysis is the key test for investigating male infertility. It is performed in compliance with...